1) Why is it important to differentiate between social anxiety disorder and autism spectrum disorder, even as a layperson?
It is important because accurate conceptualization and diagnosis informs good treatment, adjunct services, and may increase understanding from others in the individual’s life. These diagnoses can occur individually or in conjunction with one another and this would impact the course of treatment and hopefully the responsiveness of others to best support the individual. The comorbidity of social anxiety disorder is common in children with autism spectrum disorder with intellectual functioning in the average or higher range.
Currently, the diagnosis of ASD falls under the umbrella of neurodevelopmental disorder and is considered a “family of neurodevelopmental disorders” (Wöhr & Scattoni, 2013) that manifests before age three and involves “(A) Persistent deficits in social communication and social interaction across multiple contexts and (B) Restricted, repetitive patterns of behavior, interests, or activities that cause clinically significant impairment in social, occupational, or other important areas of current functioning” (American Psychiatric Association, 2013).
An ASD diagnosis includes specifying the severity level of deficits in both domains (Social Communication and Restrictive and Repetitive Behavior). Social Anxiety Disorder (or sometimes referred to as Social Phobia), on the other hand, falls under the umbrella or anxiety disorders and involves an intense fear around social scenarios where there is a perception of potential scrutiny by others.
2) How are the symptoms of ASD and SAD, on the surface, similar?
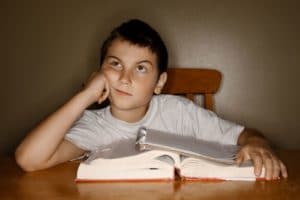
Before answering this, I want to highlight that symptom presentation looks differently in different individuals. There is proverb commonly heard in the ASD community that says, “if you have met one person with autism, you have met one person with autism” and I like this because it highlights the diversity of presentations across the spectrum. This is similar with individuals presenting with SAD, as there are a variety of different ways this may manifest on the surface, based on individual and contextual differences.
That said, some general symptoms that might be observed in both include deficits in social communication that may not be observed in more structured and individual tasks, seeming discomfort in social situations, avoidance of social connection (e.g., difficulty making or sustaining eye contact), and difficulty adjusting to changes in routine.
Without understanding the function of these symptoms, it may be difficult to differentiate between these two, and others not mentioned, diagnoses.
3) Is autism something people are born with or develop during early years?
Good question. The “cause” of autism spectrum disorder is something that is heavily research but not fully understood. While we have some evidence of genetic and environmental factors that are implicated in autism, the truth is we still don’t know what causes, or what mixture of risk factors, causes an autism spectrum disorder.
That said, it is a neurodevelopmental disorder, meaning it is something that manifests during the developmental period. This is not always the case in SAD, where the age of onset is often later in childhood-early adolescence.
4) Do people usually prescribe medications strictly for autism or more for autism plus a co-occuring issue (like anxiety, depression, ADHD, etc.)?
My experience is that psychiatrists often prescribe medications to help manage symptoms in children with autism spectrum disorder rather than for ASD itself. For instance, medications may be prescribed to help manage sleep difficulties or emotion dysregulation secondary to ASD but these medications are targeting those symptoms. Since we are often talking about young children being diagnosed (sometimes ages 2-3 years old), medications may not be recommended. Early intervention/ autism-specific therapies and any necessary adjunct services (e.g., occupational therapy, speech therapy) are often recommended as a first line of treatment.
5) If diagnosed by a psychologist, why might it be useful to see a neurologist for a second opinion or vise versa?
Autism is generally diagnosed by a psychologist or a developmental pediatrician. My belief is that families can always seek a second opinion. A specific neurology referral may be warranted where there are concerns about brain-based/organic concerns like seizures or tumors, etc.
Medically, it is best practice to refer individuals diagnosed with autism for comparative genomic hybridization (CGH), also referred to as chromosomal microarray analysis (CMA), to determine whether genetic differences are at play as this could inform additional health concerns.
6) There’s some thoughts out there that autism spectrum disorder and social anxiety disorder affect the amygdala. For example, this study implicates the amygdala and dorsomedial prefrontal cortex are affected in patients with social anxiety disorder. This study indicates preliminary analyses showed that ASD participants had stronger connectivity between the amygdala ventromedial prefrontal cortex (a network implicated in emotional modulation) and weaker connectivity between the amygdala and temporal lobe (a pathway involved in the identification of facial expressions).
What are your thoughts on this? How does that affect brain functioning and a person’s life/social interactions?
Is there a chemical imbalance with social anxiety? What is that imbalance?
I think these studies are fascinating and that the neurobiological underpinnings are critical to continue to explore as we learn more and more about the brain.
While I am not an expert specifically on the neurobiology of autism, my most recent understanding is that the structures and pathways involved are extremely complex and that despite attempts to pinpoint specific areas, research suggests that the issue is much more complex, implicating multiple areas of the social brain, along with the connecting neural networks, the cerebellum and the limbic system (Cozolino, 2014). I’ve heard about additional interest in areas including white matter, mirror neurons, corpus callosum, fusiform gyrus, right superior parietal lobule (SPL), right precuneus (Brodmann areas 5 and 7, and extending into the intraparietal sulcus) and more (Cozolino, 2014; Travers, Kana, Klinger, Klein, & Klinger, 2015). I suspect that the neurobiology of social anxiety is equally complex.
It’s also interesting to consider that a person’s environment, temperament, context, behavior, and relationships also continually shape their brain, even at a biological level. The relationship is bidirectional and fluid since we know that the brain has plasticity and can change, for better or worse. Psychotherapy, behavioral therapy, medication, and even lifestyle changes have neurobiological sequelae and lay down pathways that can become automatic overtime. As pathways become more engrained, the more difficult it may be to change them.
The theory that disorders are the result of “chemical imbalances” is tricky because of this complexity. What I have learned from my psychiatry colleagues is that psychiatric medications (the likely solution for the chemical imbalance explanation of mental illness) do work on neurotransmitters, but we do not entirely know why or if specific medications will work for a given individual.
In practice, I have seen individuals who have struggled significantly with severe anxiety, likely the result of both genetic and environmental factors, benefit tremendously after getting on medication with adjunct exposure-based therapy. Others do not benefit from medications but do benefit from in-depth psychotherapy. And some may require short-term supportive interventions.
The process of healing is one that should be collaborative and often involves trial-and-error. Hopefully, future research will tell us more and more about why interventions work from a scientific standpoint.