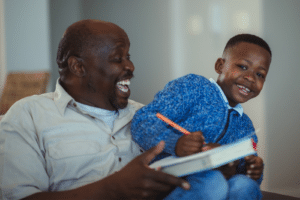
We called him “Hurricane Eric.” This tiny five-year-old with white-blond hair and big blue eyes could go from calm and placid to Category 5 in the space of a few seconds, putting both himself and his classmates at risk. I’ll never forget the first time his principal called and scheduled a meeting. Fortunately, Eric’s kindergarten teacher was his second biggest fan (after his mother), and the principal had years of experience working with neurodiverse kids.
And, fortunately, though we felt overwhelmed and afraid at first, Eric’s father and I were willing to accept that our son needed help, and we were able to trust the experts the school and our family doctor recommended. Though it took years to find the correct diagnosis and therapies that helped him, we felt like Eric’s teachers were our partners in helping him to learn and grow in the best way he could.
It doesn’t always work out like that. While parents would never take it personally if the nurse called and asked them to pick up a child with a stomach ache, there’s something different about the behavioral symptoms of brain differences.
This shorthand word stigma that is so common in mental health advocacy contains the idea that mental illness is treated as something to be ashamed of. Dr. Patrick Corrigan, a national expert on stigma and mental illness, notes, “Many people who would benefit from mental health services opt not to pursue them or fail to fully participate once they have begun. One of the reasons for this disconnect is stigma; namely, to avoid the label of mental illness and the harm it brings, people decide not to seek or fully participate in care.”
The same is true of parents whose children may need mental health care.
The fact is, people often blame parents and their children for behaviors caused by mental health conditions. When you tell a mom that something is wrong with her child or when you try to apply a stigmatizing label, it’s pretty common to see defensive behavior. For many parents, this natural position of defensiveness can be compounded by other factors.
Understand Where the Parent Is Coming From
Before you talk to a parent about their child’s possible mental health conditions or the need for testing and accommodations, it can be helpful to understand where the parent is coming from. Asking a few questions can help you orient yourself to the parent’s current attitudes and beliefs about mental illness. These beliefs can be shaped by the following:
- Personal experience
- Whether the parent knows or has interacted with someone who has a mental illness
- Cultural beliefs/stereotypes about mental illness
- Media portrayals of mental illness (for example, in television or movies)
- Past experiences (positive or negative) with healthcare institutions and barriers (such as insurance restrictions or cost)
Avoid the Blame Game
No one likes to have hard conversations. And most parents whose children have mental health conditions have an experience similar to mine. The first time they are forced to confront their child’s illness head on is in elementary school. These conversations are difficult under the best of circumstances. Because of the stigma of mental illness, parents may feel like you are attacking them or their parenting.
This initial hostile reaction is often based in fear of the unknown. A friend of mine explained why so many parents who need resources have no idea how to ask for help. “We want parents who would otherwise resist a diagnosis or label for their child to be able to access good information without being turned off by a label,” she told me. “Ideally, we can help them to steer themselves to the medical help that they need.”
This is the same concept embraced as “self-determination” for older children and adults living with mental illness. Parents want to feel like they have options. Framing the conversation in terms of help and hope, not labels, is critical to establishing trust.
Most of the time, whether they admit it or not, parents of children with difficult behaviors already worry that they are failing their children in some way. A 2016 study of how parents of children with mental health conditions view themselves demonstrated that parents whose children exhibit signs of mental illness often self-stigmatize, meaning they already see themselves as parenting failures. Reinforcing that the parent is a “good parent” and that resources and help are available is important to helping parents, especially mothers, develop and maintain positive self-esteem.
It’s also worth noting that mental illness is known to have a strong genetic component. For this reason, sometimes teachers who are seeking parental cooperation in planning what’s best for the child may find that the whole family needs additional resources. Be prepared for this conversation. Your school’s counselor can be a resource for you and help you to provide information about appropriate programs that may help.
Understand Cultural Beliefs About Mental Illness
A final barrier to parental acceptance can be cultural. A 2016 meta-analysis of how cultural perceptions and practices impacted people’s views of mental illness found that different cultures have vastly different beliefs about the causes of and treatments for mental illness.
For example, Pacific Islanders believe the source of mental illness is family conflict, while the Chinese and Nigerians see mental illness as an “imbalance of cosmic forces” that should be corrected through diet, exercise, and a focus on positive thinking. Some people even believe that demons or evil spirits cause mental illness; one of my Hispanic friends was advised by her very traditional mother to crack an egg on her son’s head to make the evil spirit leave. Many African Americans are suspicious of mental healthcare providers and prefer more informal or faith-based interventions, which is also common to Americans of all races who profess strong Christian beliefs.
Seeking out culturally appropriate guidance and resources can help you to be sensitive to the parents’ needs. The National Education Association provides a general diversity and cultural competency toolkit that can be a good place to start. The principles of cultural competency, while not specifically focused on mental health conditions, are helpful when dealing with parents who may come from a different cultural or belief system than yours.
Focus on the Goal: Helping the Child
No parent ever wants to have a hard conversation about their child’s behaviors and possible mental illness. But diagnosis, therapy, and classroom accommodations can help most children to succeed. Partnering with the parent in their child’s success can be the best solution for everyone. By understanding the parent’s attitudes and beliefs, avoiding blame, and understanding cultural differences, teachers can build trust with even the most reluctant parents.
“It’s not about the label; it’s about the services,” our son’s kindergarten teacher told us on that fateful day of our first elementary school meeting. Those services made all the difference for Eric, and they will help your students too.